Mohs micrographic surgery is the standard of care for skin cancer removals.
It was first developed to treat non-melanoma skin cancers but is now used to remove many types of skin cancer. Many surgeons are even using Mohs surgery for melanoma. It’s highly effective, tissue-sparing, and offers a quick recovery with excellent cosmetic results.
If you (or someone you care about) is considering Mohs surgery, here’s what you need to know about how it works, what it treats, surgery costs, and postoperative recovery.
How Does Mohs Surgery Work?
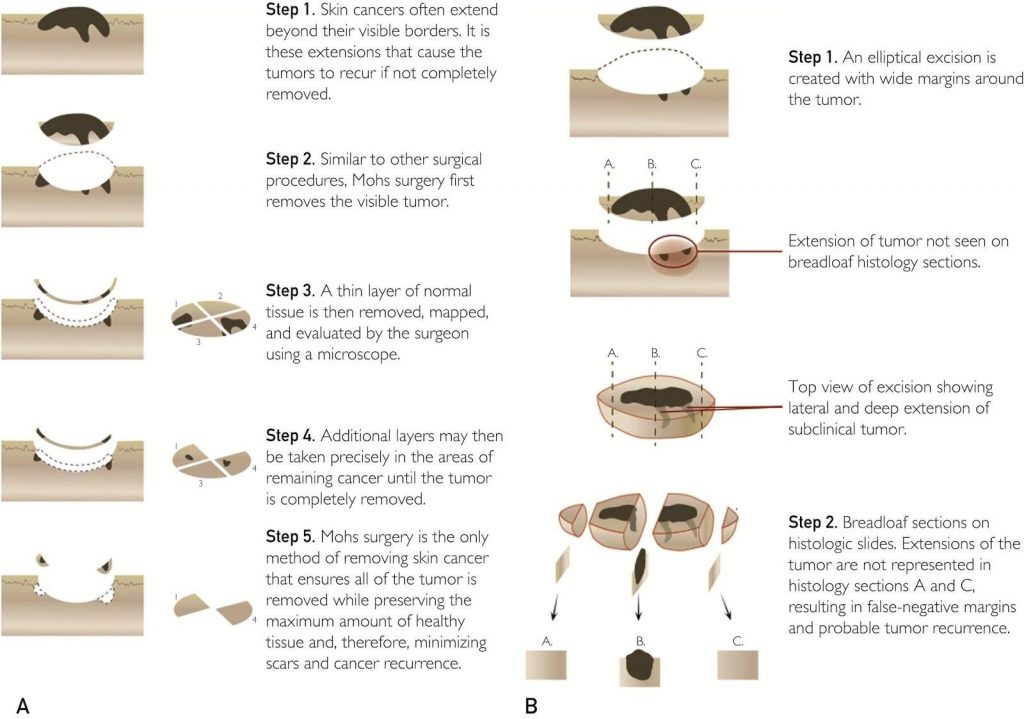
In Mohs surgery, one doctor serves as the surgeon, pathologist, and reconstructionist. The Mohs surgeon identifies and removes the visible tumor (which has already been biopsied). Then he/she removes a thin layer of tissue around the tumor to spare normal tissue.
The tissue layer is then precisely mapped out, flattened, and evaluated. The doctor examines the margins around the removed tumor — peripheral and deep — to see if any cancerous tissue remains. By doing this, they see 100% of the margin around the removed tumor. If the tumor is seen under the microscope, additional layers may be needed in only in the precise areas where the tumor remains rather than all the way around the first layer.
Why is that 100% margin so important? It drastically diminishes the chance of the cancer returning as compared to other modes of therapy.
Most skin cancer recurrences come from tumors that were not completely removed because the tumor extended beyond what the clinician could see. Skin cancers may have “roots” on or under the surface that are invisible to the naked eye. The Mohs technique greatly diminishes this possibility because it shows 100% of the margin microscopically. Since the microscope guidance allows the surgeon to completely see possible tumor extensions and irregularities, all affected areas are removed.
Before Mohs surgery and in other fields of pathology, the Breadloaf technique is used for histopathologic tumor evaluation. Surgeons would remove the tumor with a wide margin around it. Then the specimen was sent to a lab and a histotechnician would slice the tumor vertically and evaluate the selected cross-sections to evaluate the margins of the removed area.
However, only 0.1%- 1% of the tumor was evaluated in this process. They would then tell you, with some degree of certainty, whether the tumor was clear. For common skin cancers, this technique was about 90% effective, as opposed to the 99% cure rates with Mohs surgery. However, with uncommon cancers or aggressive tumors, the cure rates were as low as 30%. Now with Mohs surgery, the cure rates for those same uncommon cancers are 85-100%.
In addition, wide excision was typically done in a hospital or surgical center operating room setting under anesthesia, and patients would be sent home without having a final pathologic report on clear margins. Mohs surgery is done in an office setting, under local (i.e. lidocaine) anesthesia, with same-day margin evaluation and reconstruction. This limits the potential number of adverse events associated with general anesthesia and the inconvenience of a hospital setting.
What Types of Cancer Does Mohs Surgery Treat?
Basal cell cancer was the most common cancer treated with Mohs surgery. Mohs is now a viable treatment for a variety of common and uncommon skin cancers including but not limited to:
- Basal cell carcinoma
- Squamous cell carcinoma
- Melanoma
- Dermatofibrosarcoma protuberans
- Atypical fibroxanthoma
- Merkel cell carcinoma
- Microcystic adnexal carcinoma
- Sebaceous cell carcinoma
- Extramammary Paget disease
- Leiomyosarcoma
- Hidradenocarcinoma
- Trichilemmal carcinoma
- Mucinous carcinoma
- Porocarcinoma
- Eccrine carcinoma
Mohs surgery is a treatment option for certain stages of melanoma. Mohs surgery for melanoma in situ, which is often found on the face, allows us to remove the minimal amount of tissue while even more effectively removing the tumor. We’re even using Mohs for deeper, more invasive melanomas.
Years ago, the removal of a melanoma tumor included taking a five-centimeter margin around the tumor to best prevent recurrence. The standard excisional margins have been decreasing over the years. While abiding by standard-of-care practices, we can now take only a few millimeters around these melanomas when Mohs is done in conjunction with special stains, and the cure rates are increasing.
Will Mohs Surgery Work for Everyone and Every Tumor?
We follow appropriate use guidelines for Mohs surgery, as we would for any treatment. In 2012, a study outlined the criteria for appropriate uses of Mohs surgery. This is an evolving document and will soon be updated. In general, Mohs is deemed appropriate for:
- Head and neck tumors
- Tumors on areas that needed tissue sparing such as the hands, feet, genitalia, and shins
- Tumors with an aggressive histologic appearance
- Tumors greater than two centimeters off the head and neck
- Tumors on immunosuppressed patients, including those with organ transplants, leukemias/lymphomas, autoimmune conditions, and on immunosuppressive medications
The decision to perform Mohs surgery is ultimately a decision between the patient and the clinician. These are major factors in considering Mohs surgery as the best treatment for a specific type of skin cancer.
What Does Mohs Surgery Cost?
Mohs surgery costs change depending on the extent of the surgery and reconstruction and the patient’s insurance coverage. However, there have been studies to try to determine the averages of how much Mohs surgery costs compared to standard excisions, radiation, and cream treatments. These studies compare treatments of similar-sized tumors and consider the likelihood additional treatments in the event of recurrence. However, these studies typically do not include reconstructive costs, which may vary depending on the extent of the surgery.
The reconstruction is mainly done by the Mohs surgeon, so it’s typically performed on the same day – but the cost of reconstruction is NOT bundled into the cost of the actual Mohs tumor removal.
Mohs surgery is conducted by one surgeon who also acts as the pathologist and reconstructionist. There is typically no anesthesia, hospital, or surgical center fee. Since Mohs surgeons evaluate the entire tumor margin, the decreased risks of recurrence and metastasis also spare costs for secondary and additional treatments.
There may also be a need for a pathologist and a reconstructionist, each of whom will charge additional fees. In some cases, the use of a multidisciplinary approach by the Mohs surgeon with other doctors. For certain skin cancers, topical treatments are an option. Imiquimod cream is a treatment cream for basal cell carcinoma and other non-melanoma skin cancers. Radiation is also priced based on factions, and costs vary.
Mohs surgery is not only highly effective for skin cancer removal, it is also cost-effective as we perform the procedure in our outpatient clinics rather than an expensive hospital or surgery center. Our prices range depending on clinical factors as well as each patient’s insurance coverage. Please call our nearest clinic or billing department (512-628-0465) if you’d like an estimate of financial responsibility.
All in all, costs should not be the most important factor in selecting the right treatment option for you. Consider the overall experience, value, and final outcome.
What Can I Expect from Mohs Surgery Recovery?
Recovery after Mohs surgery depends on the tumor and the patient. I’ve had patients from very young to over 100 years old, and most patients get back to normal daily activities quickly — especially when tumors on the head and neck are removed. Level of activity, smoking, and other patient factors may affect healing time.
Sutures can be taken out in as little as one week or may dissolve. Patients can resume normal activity within one or two weeks. The scar appearance changes over time, looking significantly better in as little as a month and often fading within a year. The goal is to have a functional and aesthetically pleasing outcome.
When Mohs is done on the torso, legs, or arms, the patients need to limit their activities a little longer than for other areas to prevent sutures from spreading with movement. If non-dissolving sutures are used, I usually ask patients to keep follow-up in two weeks to allow for appropriate recovery in these areas. It’s also best to be more cautious with movement in these areas and to have appropriate limits on activity for the best outcome.
Sometimes, the surgeon may recommend small, shallow areas to heal without reconstruction. This leaves a small circular scar that fades over time. These defects require no downtime beyond the day of surgery, but they do take longer to fully heal — as little as three weeks for patients who recover quickly and as long as three months for patients with poor circulation.
What Should I Look for in a Mohs Surgeon?
Not every surgeon’s training is the same. This is true in dermatology just as it is in plastic surgery, obstetrics, and other fields of medicine. Skills and comfort levels with Mohs surgery also vary among surgeons.
Fellowship-trained Mohs surgeons have completed an American College of Mohs Surgery fellowship. These fellowships are intense programs lasting one to two years that provide dermatologists with hands-on experience in both surgery and reconstruction. In my fellowship, we dealt with 3500+ cases a year with a broad range of tumors and reconstructions. Surgeons leaving this type of program enter practice with a high level of comfort and surgical experience.
Not all dermatologists who practice the technique of Mohs surgery have done formalized fellowship training. There are societies that help with education in Mohs surgery outside of the American College of Mohs Surgery.
If you’re looking for the right Mohs surgeon for you, realize you have a choice. To make an informed decision, ask your doctor:
- What type of training have you had in Mohs surgery?
- What’s your comfort level with this procedure for this type of tumor?
- How many cases have you done in your training or practice?
- Are repairs conducted in office or sent out?
- How do your recurrence rates compare to those published for Mohs surgery?
Personally, I have experienced the level of training involved in a Mohs fellowship and would highly recommend surgeons who have completed these programs. You can check out the ACMS website to see the level of training of surgeons in your area so you can narrow your search. Again, while training varies among surgeons, skill and comfort levels in tumor types and especially reconstruction also vary.
Deciding how to treat skin cancer is no small task. Contact us today for more information about whether this is the right treatment for you.

Dr. Stan Tolkachjov is a board-certified dermatologist in Frisco and Rockwall, TX. He has a particular interest in skin cancers and rare adnexal malignancies, Mohs surgery and complex facial reconstruction, pyoderma gangrenosum, and neutrophilic dermatoses. In his spare time, Dr. Tolkachjov enjoys spending time with his family, trivia, sports, travel, and mentoring students, residents, fellows, as well as sharing ideas with his colleagues to improve patient care.